CodaMetrix stands as a transformative force in healthcare technology, pioneering autonomous medical coding solutions that address one of the industry’s most persistent challenges. This Boston-based startup has emerged from the corridors of a leading academic medical center to become a cornerstone player in the $20 billion medical coding market, fundamentally reshaping how healthcare organizations approach revenue cycle management through artificial intelligence.
Introduction and Market Context of CodaMetrix
Medical coding represents one of healthcare’s most critical yet problematic administrative functions, consuming approximately $9 billion annually across health systems while remaining notoriously manual, understaffed, and error-prone. CodaMetrix addresses these fundamental inefficiencies through its AI-powered platform that automates medical coding across multiple specialties, achieving unprecedented automation rates of over 96% while maintaining accuracy and compliance standards. The company’s solution translates clinical information into accurate sets of medical codes for patient care and revenue cycle processes, spanning from fee-for-service to value-based care models.
The healthcare industry’s administrative burden has reached critical levels, with 20-25% of U.S. healthcare spending wasted on administrative and revenue cycle tasks, making coding the most expensive component of the revenue cycle. CodaMetrix’s platform directly confronts this challenge by providing autonomous coding capabilities that enable healthcare professionals to focus on patient care rather than administrative tasks.
Founding Story and Origins of CodaMetrix
CodaMetrix’s origin story exemplifies successful healthcare innovation emerging from operational necessity. The company was founded in 2019 to refine and commercialize a Computer Assisted Coding (CAC) solution originally developed by the Massachusetts General Physician Organization’s Physician Billing Office. When existing CAC and rules-based NLP solutions proved inadequate for Mass General Brigham’s needs, the physician organizations decided to create their own solution internally.
The journey began in 2016 when Hamid Tabatabaie served as Entrepreneur in Residence at The Massachusetts General Physician Organization (MGPO), identifying opportunities for commercialization of intellectual property. This incubation period within one of America’s most prestigious healthcare systems provided CodaMetrix with unique insights into real-world coding challenges and operational requirements. The solution was initially used to code cases from multiple specialties within Mass General Brigham, demonstrating its effectiveness before commercial launch.

Michael Mercurio, who serves as EVP of Strategic Partnerships and co-founder, describes the transition from internal tool to independent company as a journey driven by the recognition that physicians “didn’t go to medical school to learn how to code”. The founding team understood that doctors needed technology to help them focus their expertise on complicated cases while automating routine coding tasks.
Founders and Leadership
Hamid Tabatabaie serves as President and CEO, bringing extensive healthcare technology leadership experience to CodaMetrix4. His background includes serving as CEO of lifeIMAGE from 2008 to 2015, CEO of Amicas from 1999 to 2005, and various leadership roles at healthcare technology companies spanning over three decades. Tabatabaie’s engineering background from Boston University, combined with his deep understanding of healthcare IT challenges, positions him uniquely to lead CodaMetrix’s mission.
Michael Mercurio, co-founder and EVP of Strategic Partnerships, maintains dual roles as Vice President of Physician Billing Services at Mass General Brigham while contributing to CodaMetrix’s strategic development. His 25-year tenure at Mass General Brigham provides invaluable operational insights and maintains the crucial connection between CodaMetrix’s technology development and real-world healthcare delivery challenges.

The leadership team has expanded significantly to support rapid growth, including Jim Whelan as Chief Revenue Officer, Tara Bradley as Chief of Staff and Customer Success, Tony Confrey as EVP of Research and Development, Evan Grossman as Chief Product Officer, and Mark Pottle as Chief Financial Officer. This executive expansion reflects CodaMetrix’s commitment to scaling transformational healthcare solutions across the industry.
Technology Platform and Business Model
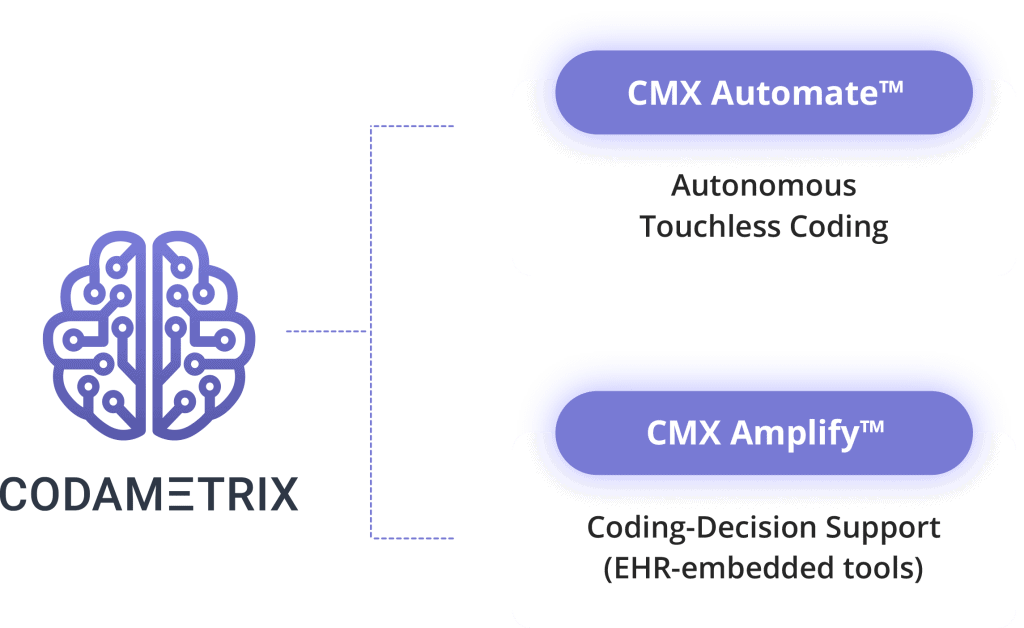
CodaMetrix operates on a Software-as-a-Service (SaaS) model, providing an AI-powered platform that combines machine learning, deep learning, and natural language processing to autonomously translate clinical information into accurate medical codes. The platform functions as a cloud-based filter that interfaces with provider networks to monitor schedules, patient demographics, orders, results, and reports.
The technology architecture emphasizes a comprehensive patient-centric longitudinal view of records, distinguishing CodaMetrix from competitors who may focus on individual encounters. When cases are complete, the system automatically predicts and assigns ICD, CPT, and modifier codes, with a quality control engine gauging predictions against confidence criteria. High-confidence cases proceed directly to billing systems without human intervention, while complex cases are routed to professional coders.
The platform’s multi-specialty capabilities span radiology, pathology, endoscopy, gastroenterology, surgery, evaluation and management, and numerous other specialties. This breadth of coverage allows health systems to implement comprehensive coding automation across their entire operation rather than addressing individual departments in isolation.
Revenue Streams and Market Performance
CodaMetrix generates revenue primarily through its SaaS platform licensing model, serving a medical coding market valued at approximately $20 billion annually. The company processes well over 100 million clinical documents annually, spanning multiple service lines while enriching them with key data including registration, scheduling, orders, and medications to ensure optimal coding accuracy.
Customer performance metrics demonstrate substantial value creation: providers utilizing the CodaMetrix platform experience a 60% reduction in coding costs, 70% reduction in claims denials, and a 5-week acceleration in time to cash. These improvements translate directly into significant revenue recovery and operational efficiency gains for healthcare organizations.
The platform currently serves more than a dozen premier provider organizations and health systems, representing over 200 hospitals and 50,000 providers. Notable customers include Mass General Brigham, University of Colorado Medicine, Mount Sinai Health System, Yale Medicine, Henry Ford Health, University of Miami Health System, and UMass Memorial Health.
Funding Rounds and Financial Growth
CodaMetrix has demonstrated strong investor confidence through two major funding rounds totaling $95 million. The Series A round in February 2023 raised $55 million, led by SignalFire with participation from Frist Cressey Ventures. This substantial initial round reflected investor recognition of the company’s market potential and proven technology.
The Series B round in March 2024 secured an additional $40 million, led by Transformation Capital with continued support from existing investors SignalFire and Frist Cressey Ventures. Todd Cozzens, Co-Founder and Managing Partner at Transformation Capital, joined CodaMetrix’s Board of Directors as part of this investment.
These funding rounds support CodaMetrix’s expansion plans, including advancing AI-powered solutions, enhancing medical coding quality, producing clinically comprehensive datasets, and reducing overall healthcare costs. The financial backing enables continued platform development, market expansion, and team growth to meet increasing demand for autonomous coding solutions.
Competitive Landscape and Market Position
CodaMetrix operates in a competitive landscape populated by several notable players, each approaching medical coding automation from different angles. Primary competitors include Nym (founded 2018, New York), which focuses on automated medical coding processes using clinical language interpretation. Fathom (founded 2015, San Francisco) specializes in AI-driven medical coding automation with services including production coding, backlog processing, and real-time audits.
Other significant competitors include Maverick Medical AI (founded 2018, Tel Aviv), which utilizes deep learning and synthetic data generation for medical coding; Synaptec Health (founded 2018, San Francisco), offering automated medical coding software with minimal human intervention; and XpertDox (founded 2015, Arizona), providing AI-powered coding solutions focusing on accuracy and claims processing.
Competitive Advantages and Market Differentiation
CodaMetrix maintains several distinctive competitive advantages that position it favorably in the medical coding automation market. The company’s origin within Mass General Brigham provides unparalleled real-world validation and operational insights that competitors developed outside healthcare systems may lack. This healthcare system pedigree ensures the platform addresses actual operational challenges rather than theoretical problems.
The platform’s multi-specialty autonomous coding capability distinguishes CodaMetrix from competitors who may focus on specific specialties or require more human intervention. The company’s automation rate exceeding 96% across specialties represents industry-leading performance. Additionally, CodaMetrix’s Epic Toolbox designation and deep EHR integration capabilities provide seamless implementation advantages.
Recognition by KLAS Research as the number one solution in the “Reduce Cost of Care” category validates CodaMetrix’s market position and customer satisfaction. The platform’s real-time audit capabilities and feedback loops enable continuous AI learning improvement, creating a sustainable competitive moat through accumulated data and algorithmic refinement.
Industry Recognition and Awards
CodaMetrix has achieved significant industry recognition that validates its market position and growth trajectory. Forbes ranked the company as the second-best startup employer in America among 3,000 companies, reflecting strong leadership and team dedication. This recognition demonstrates CodaMetrix’s success in building an exceptional organizational culture alongside technological innovation.
The company’s KLAS Research recognition as the top solution for reducing cost of care provides crucial third-party validation in the healthcare technology market. KLAS ratings carry substantial weight in healthcare purchasing decisions, making this recognition a significant competitive advantage.
Future Vision and Market Impact
CodaMetrix envisions a future where medical coding becomes a largely autonomous function, enabling healthcare professionals to work at the top of their licensure with greater satisfaction and reduced administrative burden. The company’s long-term vision extends beyond billing applications to include critical support for clinical decision making, research, population health, and public health initiatives.
The platform’s ability to transform claims data from “notoriously unreliable to clinically valuable” represents a fundamental shift in how healthcare organizations can leverage coding data for operational and clinical insights. This transformation potential positions CodaMetrix as more than a cost-reduction tool, establishing it as a platform for healthcare intelligence and decision support.
As healthcare continues its digital transformation journey, CodaMetrix’s autonomous coding platform addresses one of the industry’s most persistent administrative challenges while creating new possibilities for data-driven healthcare improvement. The company’s strong foundation, proven technology, substantial funding, and strategic market position suggest continued growth and market impact as healthcare organizations increasingly adopt AI-powered solutions to enhance operational efficiency and clinical outcomes.
Also Read: Calendly: Founders, Business Model, Funding, Revenue
To read more content like this, subscribe to our newsletter